Breast Implant Illness and What You Need to Know (Part 2)
This is Part II of my breast explant journey and if you missed Part 1, you can go back and read it here.
I waited until January reach back out to the surgeon’s office to see about scheduling the surgery.
I had been putting off the surgery date because my husband was going through a job transition and wanted to make sure all his ducks were lined up before I threw this in the mix. At least that’s what I told myself.
Truly, deep down, I was scared.
What if my symptoms have nothing to do with my implants?
What if I have nothing to even put into a bra?
Will my recovery be super painful?
God, those drains.
Will my nipples shrivel up like charred raisins?
What if I get a blood clot? An infection?
Will I look like I was attacked by a shark?
All of these thoughts and some much more dramatic passed through my mind after my consult. The unknown was scary but then keeping them in was scarier. I was aging faster than my real age (had that tested), I was in pain, my old health issues were starting to come back from the grave, and my blood tests showed that the elevated levels of estrogen in my breast tissue. Based on all the things I had been reading in both the FB group and various articles, I couldn’t dismiss the connections.
I had always believed that I would replace my implants with newer ones at the 10 year mark. Well that came and went and thank God for my procrastination. It was in my 11th year of having implants that I learned about BII. Finally! My procrastination actually worked in my favor!
So when I called, they said he had an opening in two weeks. I knew if I waited any longer, I was going to be out of commission for spring break and the start of my boys’ baseball seasons. Waiting was not an option anymore for so many reasons.
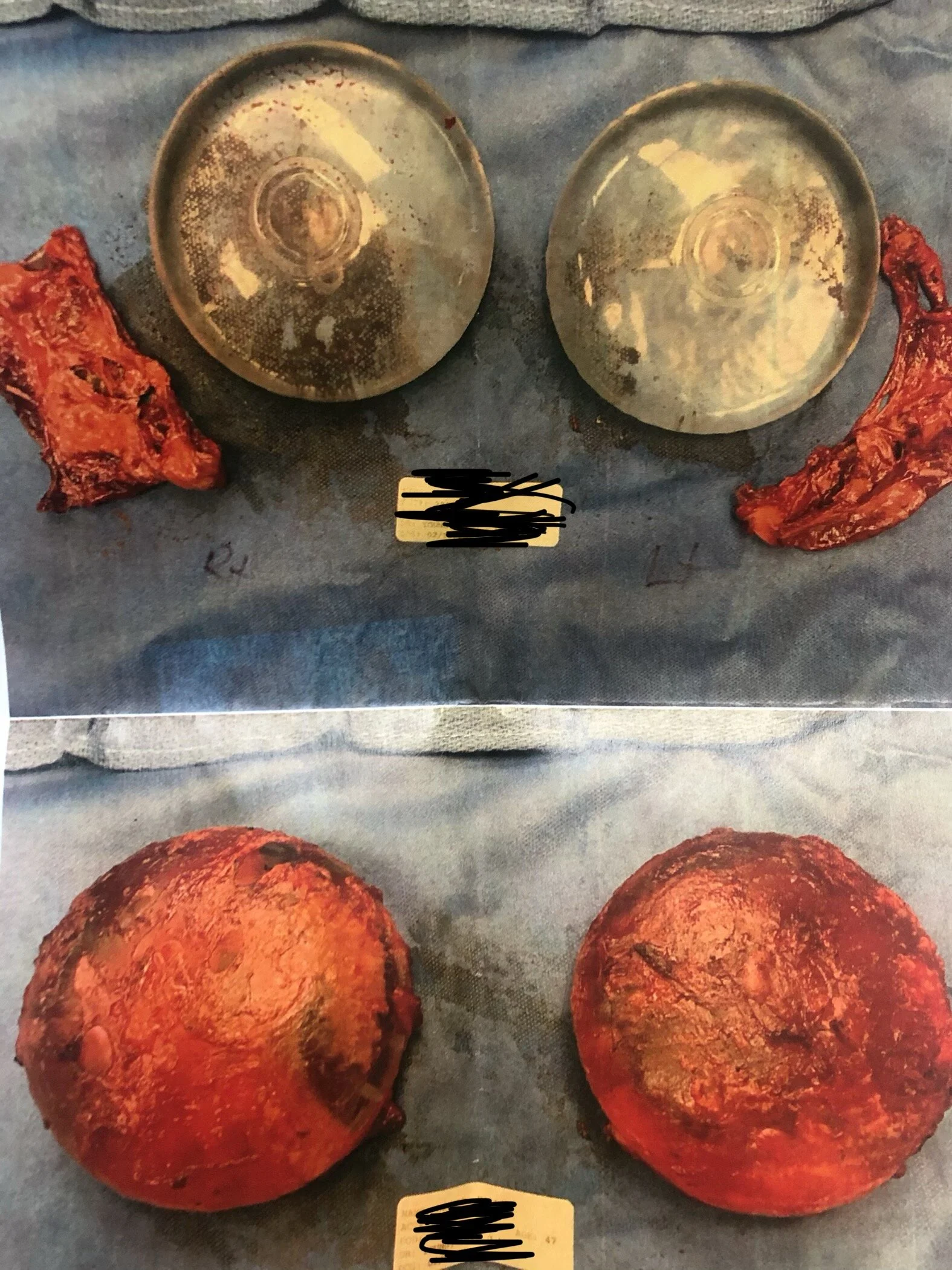
I went in for a pre-surgery consult a few days before surgery to take pictures, turn in consent forms and make the final payments. I chose to do a lift at the same time as well as a total capsulectomy because I wanted to get rid of the guaranteed excess skin I was going to have as well as all of the tissue that surrounded the implant in case of any infection. I explained that I also wanted those capsules to be sent to pathology for testing for a bacteria, abnormalities, cancer cells, infections, etc.
In the two weeks since scheduling, I researched recovery protocols other women used with success and stocked up on my recovery tools/necessities. I did all my laundry and made sure I had zip up sweatshirts, button up shirts, a compression bra and bras with no underwire.
The tools I’ve used or will use for my recovery:
Gauze to use as padding around incisions and drains
Skin healing essential oils: geranium, helichrysum, myrrh, bergamot, copaiba, spikenard, and Immortelle blend (dōTERRA)
Digestion and bloating support: DigestZen (after surgery, they said to expect bloating and they were right.)
Essential oils/supplements for immune, detox, and pain support: OnGuard, Tea Tree, Zendocrine, Aromatouch, and Deep Blue capsules
Correct-X ointment (dōTERRA) for incisions once steri-strips come off
Organic greens powder or capsules - alkalize and detox the bod
Carrot Juice powder - repairs and tones the skin, helps with circulation, as well as source of antioxidants
Beets powder - helps with detox, circulation, a rich source of iron,
Fiber - keep things moving post-surgery (anesthesia, pain meds, etc.)
Liposomal C - vitamin C delivered under the tongue for maximum absorption and supports immune system, cell health, growth and repair of tissues
Fanny pack to hold drains
Silicone straws to drink hot liquids without having to tip your mug
CBD - addresses anxious feelings and provides mood lift.
Sleep support (bed wedge like these) to keep upper body elevated during sleep. I have an adjustable bed and was awesome on my back.
Bone broth - great nutritional support when I didn’t feel like eating
Post-surgery was as expected—groggy and a little uncomfortable. Pain meds were on board and the nurse gave me another before I left to go home. I took them again that night and again the next day and night. After that, I was able to control the pain. I used ibuprofen once then switched to my doTERRA supplements like Copaiba, Deep Blue and CBD. I use copaiba to support healthy tissues, inflammation, and calm me down. CBD encourages the body to use its own cannabinoids while Copaiba attaches directly to endocannabinoid receptors. You can read more about these two supplements here and here.
There are drains that come from under the armpit area which are taped down to your body. The tubes are about 18” to 24 “ long and require you to safety pin the drain bulbs to your compression bra or ace bandage that is wrapped around your chest. I found that using a fanny pack was much more comfortable and kept them out of the way.
I spent the first couple of days in bed and only got up to use the restroom. On day 3 (I consider surgery as my day 1), I was able to do more and able to make some food as well as take my first shower which is recommended 48 hours post surgery. It wasn’t easy but it was definitely needed as it brought me back to life.
Pre-surgery
The hardest part was the buildup to the shower. I was afraid of what it everything looked like under all the gauze and bandages and it was all for nothing. I was pleasantly surprised at my shape and most of the gross was covered by the steri-strips. We have a walk in shower with a bench which was super helpful. I was able to sit down and process it all, feeling the safety of the bench in case it made me light-headed. I’m not the nurse in the family—that’s my husband. I’m the nutritionist and therapist. We all have our limits and blood/trauma are mine.
The reason I was nervous was because my family wasn’t home to help on day 3 through day 7. We had a quick trip planned to Copper Mountain in Colorado for Presidents’ Day weekend and I messed up plans by scheduling surgery when I did. But again, time was not on my side and I had to. My mom and sister popped over to check on me and bring me anything I may have needed (I didn’t because look at my list!) but it was weird to be alone. I had to get my own food and drinks but I prepared by having easy to prepare meals and drinks/mugs/glasses/plates ready on the counter.
However, on the flip side of that, it was kind of nice to be alone. No kids to nag or worry about and I was able rest without interruption. Only one I had to keep alive was the dog and he’s low-maintenance at this point.
As far as physical restrictions go, I am not allowed to lift my arms over my shoulders so everything is done with T-Rex arms the first few days. Then after that I could reach out a little further but still nothing that required pushing or pulling. As the pain subsides, it’s easy to forget that part so I have to always think about the stitches. If I push and pull, those stitches pull apart and then my scar will be bigger. Also, when I push and pull, I use chest muscles which we don’t want to do during this healing time. The doctor explained to me that when the chest muscles move up and down when it’s in a state of trauma like this, fluid can get in behind the muscle which can cause infection.
Each day I empty the drain bulbs and record the number of ccs in each. I had a follow up consult six days after surgery and I was still draining too much to have them taken out. The goal is to get to less than 5 ccs on each side before the drains can come out and I’m on day 11. This has been the worst part of it, honestly. It’s uncomfortable, gross, there’s no great way of concealing them well, and I worry that I’ll accidentally snag a tube on something. At the consult, I got a picture of my implants with and without the capsule.
The goal is to keep fluid low over this weekend and get these babies out on Monday so fingers crossed. Once they’re gone, it’s slow and steady into regular activity. At two weeks post-surgery they say some light cardio is okay and I’ll be able to resume normal activity at 6 weeks.
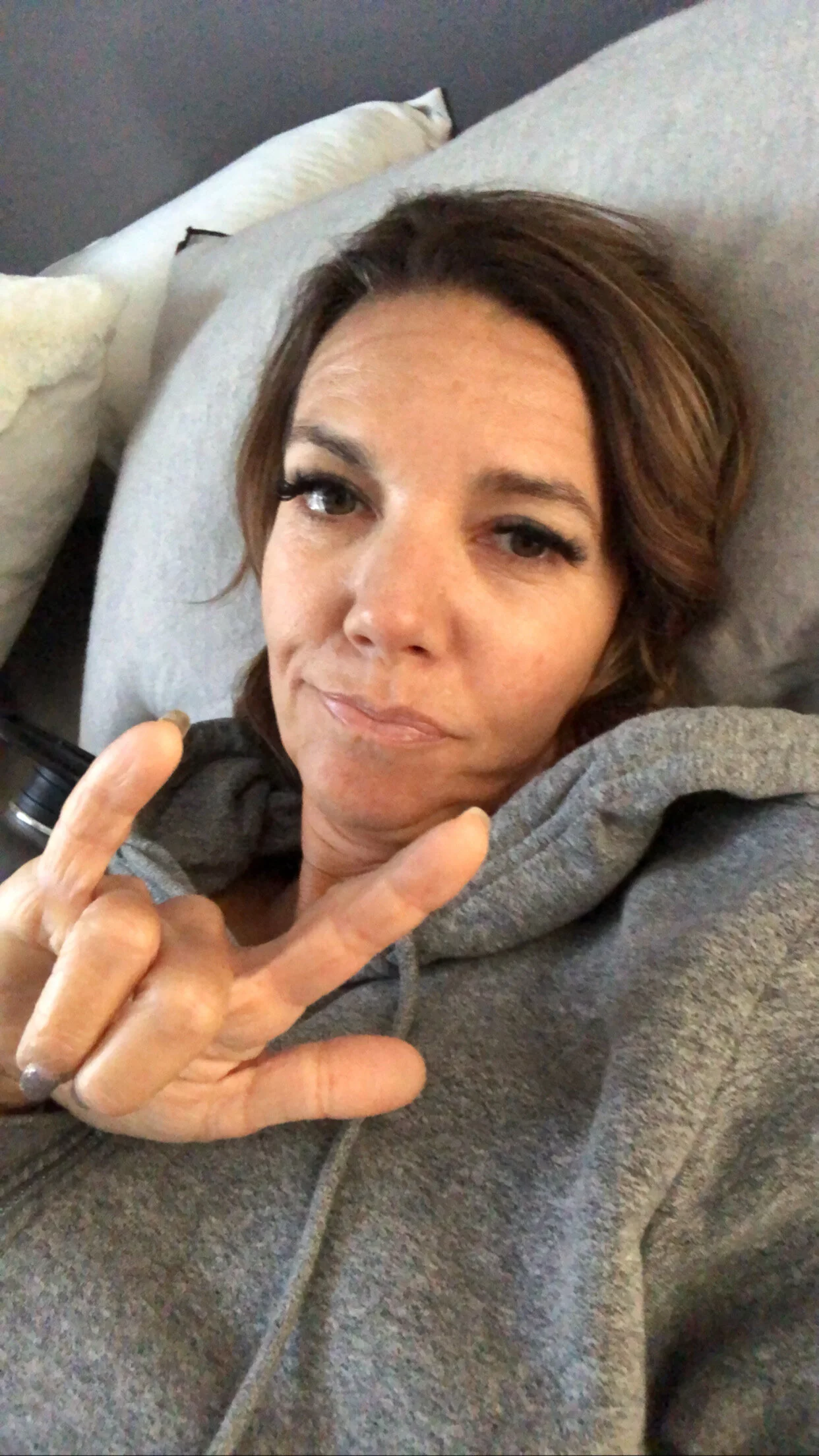
At home, day 3 of recovery
But with all the work that clearly goes into getting these implants out, I’m VERY happy they’re gone. They were a ticking time bomb and I was already starting to feel the damage. As of today, I’ve had zero joint pain and my back pain hasn’t flared up.
What’s been important in this whole decision is that I focused on what I’d be gaining, not what I was losing. I’m gaining joint mobility, a healthy back, a higher quality of life, freedom from worry, and, hopefully, years to my life. I think that’s worth any pain I may be going through now.
I look down and even though I was with implants for 12 years, I see the real me. I feel like me. And that feels awesome.
Again, I cannot express enough that this information needs to be shared. Let your gal pals know what’s up and if someone is thinking about getting implants, it’s important they know ALL the risks. I’m not here to tell anyone to not get implants or to schedule their explant surgery ASAP but to inform through my own experience. I want to help bring awareness to what BII is and what symptoms to look for because so many women are misdiagnosed or told it’s just their age and what comes with the territory.
Thanks for reading and sharing with the people you love.
xo,
Hal